Treatment of Colorectal Cancer
Colon cancer is the second most commonly occurring cancer in women, and the third most commonly occurring cancer in men. There were over 1.9 million new cases worldwide in 2020. Of these 1.9 million cases of cancer in the colon, approximately 500,000 are located in the rectum, the lowest segment of the colon. The following information is specific to the treatment of rectal cancer.
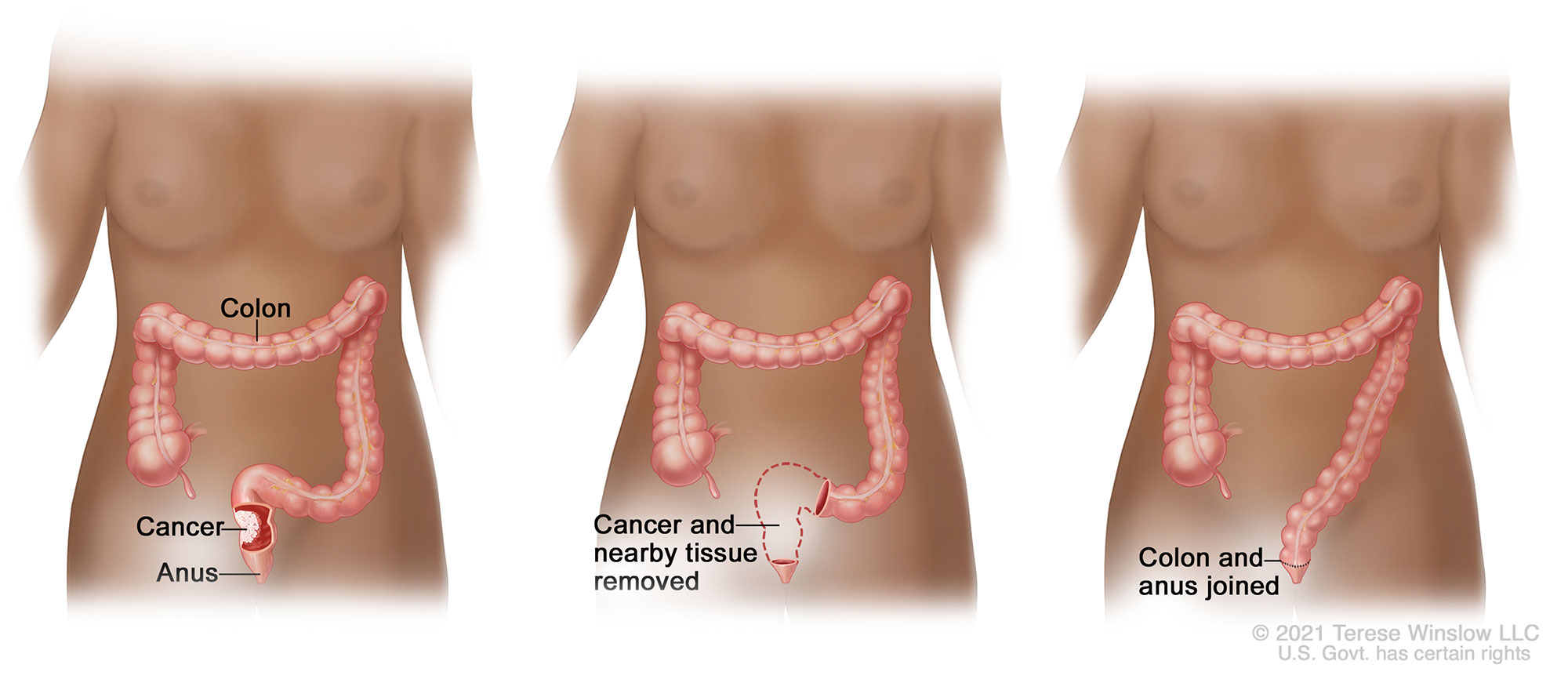
Treatment of rectal cancer most often involves radiation and chemotherapy followed by surgical removal of some or all of the rectum. The colon is then reconnected to the remaining rectum or anus with surgical staples or sutures; this connection is called an anastomosis.
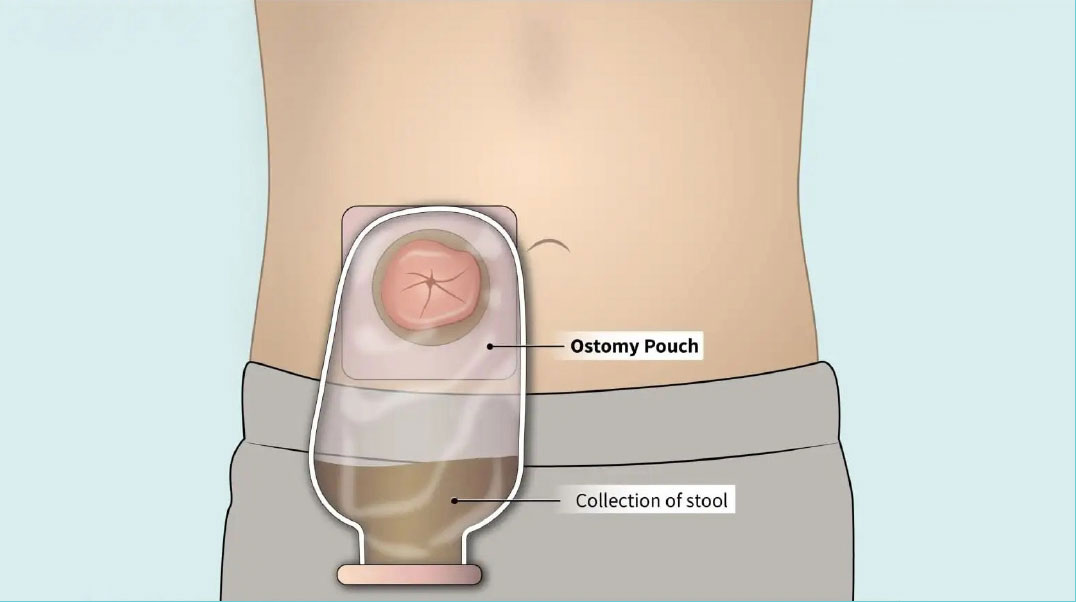
Because the risk of incomplete healing of the colon anastomosis is high, and the consequences could be dire, the surgeon may also create an ostomy (also called a stoma), which temporarily diverts the stool away from the healing anastomosis to the outside of the body and into an ostomy bag. Usually the ostomy is needed only until the rectum has healed, and then it can be reversed. If the entire rectum is removed, however, the ostomy may be permanent.
If the ostomy is intended to be temporary, the patient typically keeps the ostomy for approximately 2-9 months. The eventual reversal of the ostomy requires another operation, with a second hospital stay and recovery period.
Resection of the Rectum with Anastomosis
As with any surgery, complications can develop. While an ostomy procedure after rectal resection surgery is the current standard of care to provide protection to the healing anastomosis, specific risks are associated with the ostomy operation. The most common of these complications may include:
- Dehydration
- Irritation and inflammation of the skin around the ostomy
- A hernia at the site of the ostomy
Additionally, complications may develop from the secondary surgery 2-9 months later to reverse the ostomy.
In addition to physical complications, ostomy patients may experience an impact to their quality of life, due to:
- Social isolation
- Reduced physical activity and/or intimacy
- Extended recovery after cancer surgery
- Added expense of ostomy supplies
About Colovac1
Colovac is a colorectal anastomosis protection device intended to reduce the contact of fecal content at the anastomotic site following colorectal surgery. The device is placed at the time of the rectal resection surgery and is fully reversible. Colovac is designed to remain in place for 10 days, until the body’s natural healing and tissue repair processes are complete, after which it is removed during an endoscopic procedure similar to a colonoscopy, without the need for a second surgical intervention.
For the majority of patients, Colovac is expected to eliminate the need for a second surgery. This enables patients to resume normal activity after their cancer resection surgery without the stigma and complications associated with an ostomy procedure. Colovac is an investigational device, not currently available for sale. A multi-center clinical trial is underway to evaluate the safety and effectiveness of Colovac as an alternative to temporary diverting ostomy.
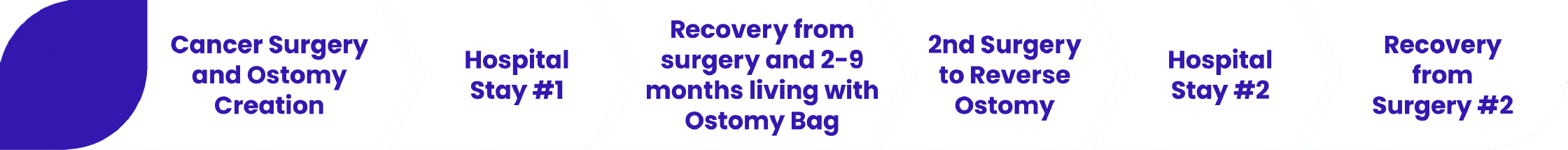
Rectal Cancer Treatment without Colovac
- Time to Full Recovery: 2-9 months
- 2 Surgeries, 2 Hospital Stays
- Risk of Complications
- 2 Surgeries Under Anesthesia
- Additional Incisions
- Ostomy Complications
- Risk of Permanent Ostomy
- Quality of Life Due to Ostomy Bag
- Social Isolation
- Impact to Physical Activity and Intimacy
- Added Expense of Ostomy Supplies
- Cost to Patient and Health Care System
- Multiple Surgeries and Hospital Stays
- Time to Full Recovery

Rectal Cancer Treatment with Colovac
- Time to Full Recovery: as little as 2 weeks
- Only 1 Surgery and Hospital Stay
- Risk of Complications
- Single Surgery under Anesthesia
- No Ostomy Complications
- Patient Satisfaction
- No Ostomy Bag, No Lifestyle Changes
- Faster Return to Normal Life
- Decreased Cost to Patient and Health Care System
- Single Surgery and Hospital Stay
- Reduced Time to Full Recovery
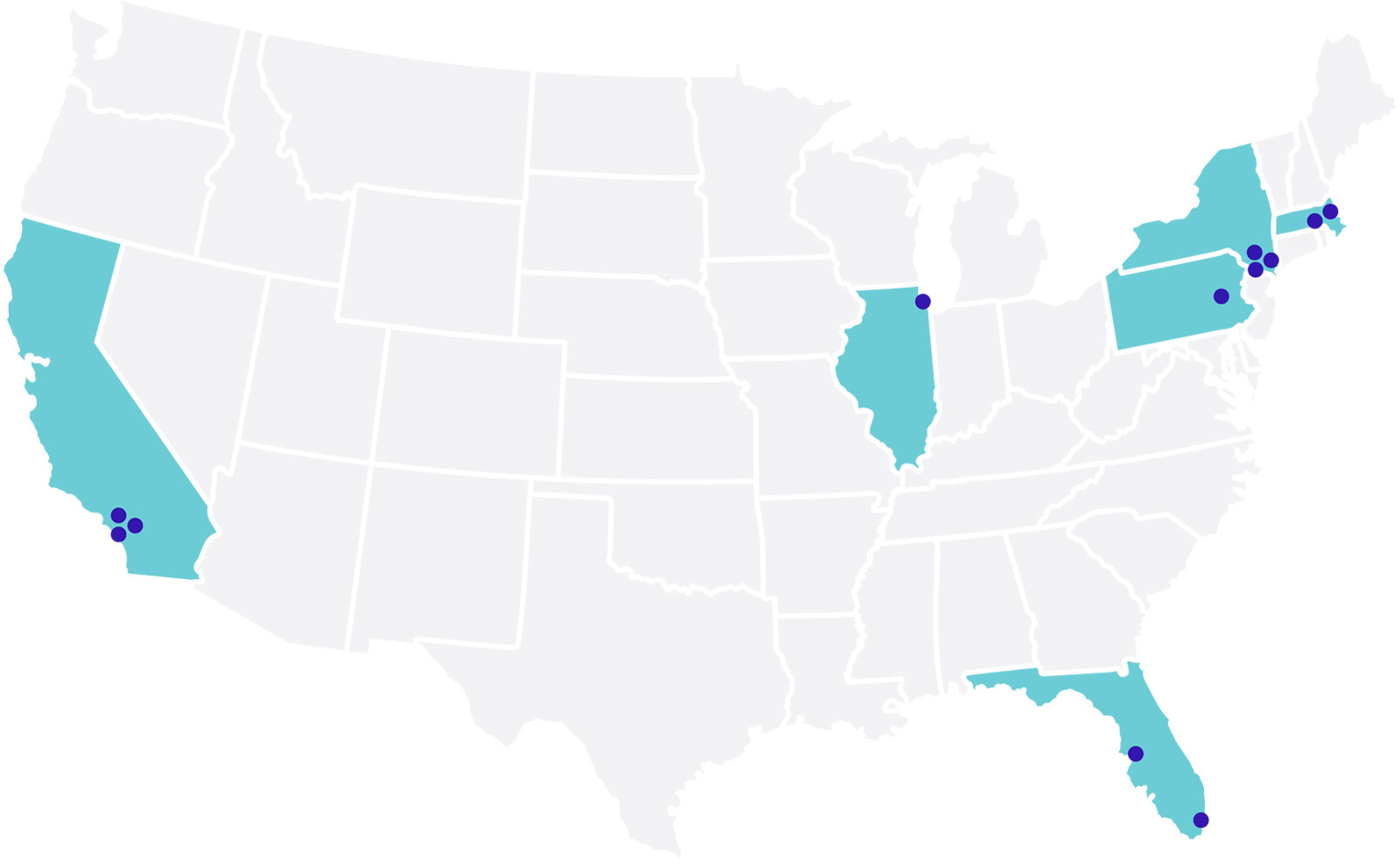
About the Colovac Clinical Study
Following successful pilot studies in Europe in which the majority of patients avoided an ostomy, SafeHeal is preparing to enroll patients in a larger clinical study at up to 25 leading academic medical centers in the United States and Europe. The aim of the SafeHeal study will be to assess the potential for patients with rectal cancer to safely avoid an ostomy in favor of a novel device, the Colovac colorectal anastomotic protection device.
- Colovac Potential Benefits
- Patients may avoid an ostomy
- No second surgery and hospital stay
- Faster return to normal life
You may be eligible to participate in the Colovac study if you:
- Are 18 years old or older
- Are undergoing a rectal cancer resection with a planned diverting ostomy
Watch this space for updates on the Colovac clinical study.
Clinical Partners:
United States
California
Cedars-Sinai Medical Center
Los Angeles, CA
 Karen Zaghiyan, MDCONTACT: Gayane Ovsepyan
Karen Zaghiyan, MDCONTACT: Gayane OvsepyanResearch & Education Program Coordinator
Gayane.Ovsepyan@cshs.org
(310) 289-9224
Kaiser Permanente Los Angeles
Medical Center
Los Angeles, CA
Keck Medicine of USC
Los Angeles, CA
 Sang Lee, MDCONTACT: Valentina Rodina
Sang Lee, MDCONTACT: Valentina RodinaClinical Research Coordinator Supervisor
Valentina.Rodina@med.usc.edu
(323) 394-0756
Florida
Tampa General Hospital
Tampa, FL
University of Miami Medical Center
Miami, FL
 Nivedh Paluvoi, MDCONTACT: Erick Ponce
Nivedh Paluvoi, MDCONTACT: Erick PonceClinical Research Coordinator
exp554@miami.edu
(305) 243-7298
Illinois
Northwestern University
Chicago, IL
 Scott Strong, MDCONTACT: Sharnia Lashley
Scott Strong, MDCONTACT: Sharnia LashleyClinical Operations Manager
sharnia.lashley@northwestern.edu
(312) 926-0159
More
Massachusetts
Boston Medical Center
Boston, MA
 Jennifer Davids, MDCONTACT: Kate Cilley
Jennifer Davids, MDCONTACT: Kate CilleyResearch Coordinator
Katherine.Cilley@bmc.org
(617) 414-8092
UMASS Memorial Medical Center
Worcester, MA
 Justin Maykel, MDCONTACT: Samuel Feinberg
Justin Maykel, MDCONTACT: Samuel FeinbergClinical Research Coordinator II
Samuel.Feinberg1@umassmed.edu
(508) 334-4918
New York
Lenox Hill Hospital
New York, NY
 Joseph Martz, MDCONTACT: Sasha Suarez, MD
Joseph Martz, MDCONTACT: Sasha Suarez, MDClinical Research Coordinator
SSuarez3@northwell.edu
(212) 434-4350
Maimonides Medical Center
New York, NY
 Rebecca Rhee, MDCONTACT: Gene Sobol
Rebecca Rhee, MDCONTACT: Gene SobolDirector, Performance Improvement
GSobol@maimonidesmed.org
(718) 283-7926
Mount Sinai Hospital
New York, NY
 Patricia Sylla, MDCONTACT: Roxanne Mistry
Patricia Sylla, MDCONTACT: Roxanne MistryClinical Research Coordinator I
Roxanne.Mistry@mountsinai.org
(212) 241-0492
New York Presbyterian-Weill Cornell Medical Center
New York, NY
 Dorna Jafari, MDCONTACT: Rohit Rasane
Dorna Jafari, MDCONTACT: Rohit RasaneClinical Research Specialist
rkr4004@med.cornell.edu
(646) 962-2789
Pennsylvania
Main Line Health System
Philadelphia, PA
 John Marks, MDCONTACT: Desirae Chandran
John Marks, MDCONTACT: Desirae ChandranOncology Clinical Research Coordinator I
ChandranD@mlhs.org
(484) 476-2395
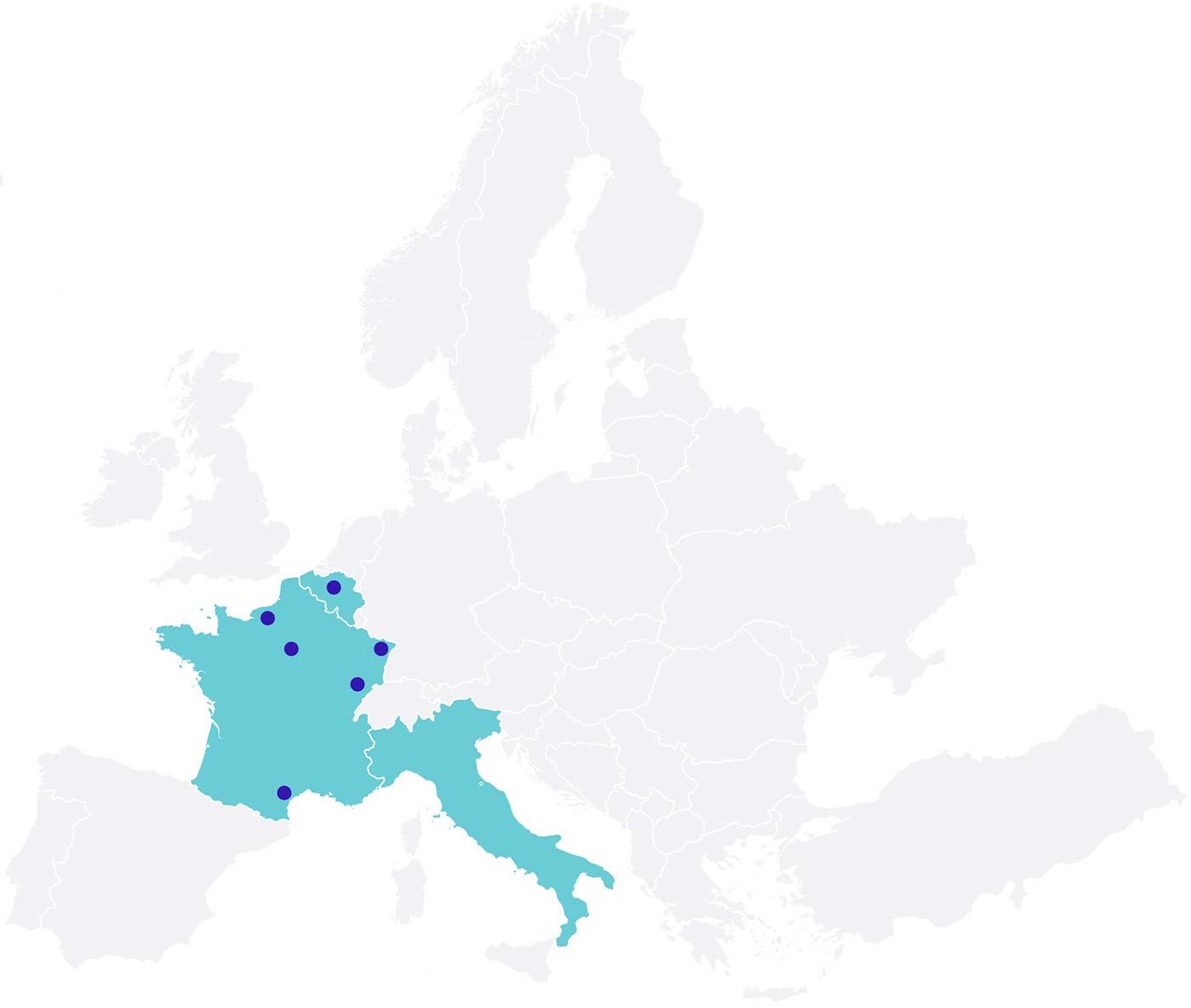
Europe
Belgium
Antwerp University Hospital
Edegem, Belgium
France
Bordeaux Colorectal Institute Clinique Tivoli-Ducos
Bordeaux, France
CHU de Rouen
Rouen, France
Hôpital Saint-Antoine AP-HP
Paris, France
Hôpital Saint-Louis AP-HP
Paris, France
IHU Institut Hospitalo-Universitaire de Strasbourg
Strasbourg, France
Italy
Istituto Clinico Humanitas
Milan, Italy
1 Colovac is an Investigational Device, Limited by Federal (or United States) Law to Investigational Use.
V8.3_06142024





 Elisabeth McLemore, MDCONTACT: Andrew Oh
Elisabeth McLemore, MDCONTACT: Andrew Oh Jorge Marcet, MDCONTACT: Avennette Pinto
Jorge Marcet, MDCONTACT: Avennette Pinto Prof. Niels Komen
Prof. Niels Komen Prof. Quentin Denost
Prof. Quentin Denost Prof. Jean-Jacques Tuech
Prof. Jean-Jacques Tuech Prof. Jérémie Lefevre
Prof. Jérémie Lefevre Prof. Léon Maggiori
Prof. Léon Maggiori Prof. Didier Mutter
Prof. Didier Mutter Prof. Antonino Spinelli
Prof. Antonino Spinelli